Bringing this post back for this month’s Down Wit Dat T21 Blog Hop
—–
I’ve been thinking and reading a lot about anxiety recently. When I was diagnosed with Asperger’s, I was also diagnosed with Social Anxiety Disorder.
Here’s how I feel about that: Social Anxiety? Yes. Disorder? Not so much.
Disorder implies that my social anxiety is irrational. Is it? Consider this:
“Anxiety at appropriate levels is important for adaptive functioning. There are many environmental hazards that must be avoided and these are often learned through the process of anxiety induction. The resultant anxiety response is learned through the association of certain stimuli with unpleasant consequences.” (from “Autism and the Physiology of Stress and Anxiety”, Romanczyk and Gillis)
Anxiety, like fear, protects us from danger. It raises our guard and makes us wary. In this way, it’s healthy. Without it, we might be less motivated to get an education, to work, to care for our loved ones and ourselves.
What is Anxiety?
Anxiety is a state of worry, concern or dread related to something that hasn’t yet happened and may, in fact, never happen. Think about some things that we typically feel anxious about:
- committing to a relationship
- giving a major presentation for school or work
- becoming a parent
- meeting a partner’s family
- starting a new job
- learning to drive
- flying on an airplane for the first time
- traveling in a high crime area
When you feel anxious about an upcoming event, you spend more time thinking about it and preparing for it than you would for a more mundane activity. You examine the possible consequences and give extra attention to your actions to ensure the best possible outcome. Anxiety heightens your awareness; heightened awareness sharpens your focus, increasing your safety.
It’s important to note that here and throughout this piece, when I talk about anxiety, I’m referring to appropriate levels of anxiety, not paralyzing anxiety. An appropriate level of anxiety is one that is manageable. I feel nervous in the days before giving an important Powerpoint presentation, but I manage my anxiety and complete the presentation to the best of my ability. An inappropriate level of anxiety is one that prevents a person from completing a necessary or desired activity. For example, if I got so anxious about the presentation that I ended up sick in bed, fainted in the conference room, or lied to avoid presenting.
Not all anxiety is healthy and it’s important to recognize where your anxiety falls on the healthy/unhealthy continuum.
The Function of Social Anxiety in ASD
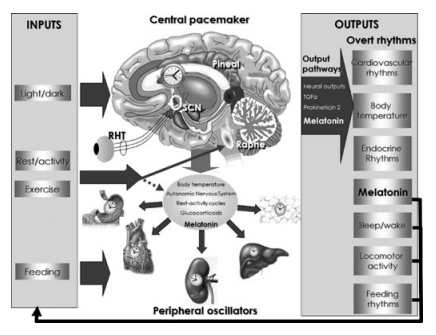
So that’s how anxiety works in the typical brain. But what about in the autistic brain?
From childhood, autistic people know that we’re missing key information in social situations. We often have difficulty interpreting facial expressions, tone of voice, body language, and non-concrete speech. Some people also struggle with auditory processing and sensory overload in public or group settings.
The results of our social communication challenges can range from inconvenient (missing a joke or not following a conversation) to dangerous (being bullied, taken advantage of or assaulted). There are also negative health consequences–many autistic people need hours or days to physically recover from prolonged or intense social interaction.
Over time, “through the process of anxiety induction,” we realize that certain social situations are “environmental hazards that must be avoided” (as Romanczyk and Gillis described). In other words, because of a very real hazard, we develop anxiety that for us has a very real cause. It isn’t disordered. It’s a defense mechanism, developed through “the association of certain stimuli with unpleasant consequences.”
Social anxiety is, therefore, not only “important for adaptive functioning” in autistic people, it’s essential.
 Red Light, Green Light
Red Light, Green Light
Autistic social anxiety is not the same as neurotypical social anxiety. If a person with intact social communication abilities has severe anxiety about social situations, then they have a disorder because their fear is irrational. When a person with impaired social communication abilities has anxiety about social situations, they are like a poor swimmer who is anxious about boarding a boat. The perceived risk is real and rational.
If fear is a red light–a glowing “stop” signal in our brain–then anxiety is a yellow light. It’s the feeling that says, “slow down, caution, stop and pause a moment before continuing down this road.”
We should heed this feeling, not cure ourselves of it.
Appropriate vs. Inappropriate
But, some will say, too much social anxiety and you’ll become a recluse! A hermit! The little old lady shouting at those darn kids to get off her lawn!
Well, yes and no. First of all, allow me to horrify the more socially oriented among you by saying this: people aren’t all that interesting and the rewards of socializing are sometimes overrated. Consider the possibility that all of the following (fictional) people are meeting their needs for social interaction:
- the person who lives alone, works at home and in the evening participates in role-playing games, an acting workshop and a drumming circle
- the person who lives with a partner and has lunch once a week with a close friend
- the person who attends classes full-time and prefers to socialize online in text-based formats outside of class hours
- the person who chooses to spend time at home with family and only goes out for necessary errands or events
- the person who works around people all day and likes to spend their evenings alone
The social preferences of these people may differ from the majority of their peers, but they aren’t exactly in Grey Gardens territory.
Being anxious about socializing is not the same as completely avoiding social situations. It’s possible to manage social anxiety in the same way we manage anxiety about other things. Someone–NT or autistic–might feel anxious about starting a new job, but that doesn’t mean they won’t do it. Most people have strategies for managing anxiety and autistic people are no different.
What is different is that our social anxiety is automatically pathologized and then “treated” with therapy or medication. We’re told that our fear is irrational and we need to change the way we “think about” social interaction. We’re told that if we just “relax a little” we’ll find social interaction much more enjoyable.
What would be far more helpful is to acknowledge our anxiety as valid and support our right to socialize at our preferred level, in our preferred ways, without being stigmatized for it.
What Anxiety Tells Us
So how does social anxiety keep us safe?
First there is the obvious example: when you have difficulty interpreting nonverbal cues, it can be hard to know when another person is a threat. This can be especially true for autistic women and girls, increasing our chances of becoming the target of sexual assault, sexual abuse or domestic violence. The autistic woman who feels anxious about dating, intimate relationships or venturing into unfamiliar situations has good reason to–the statistics for violence against autistic women are alarming.
Autistic people are also often victims of bullying. The autistic boy or girl who is anxious about recess or the school bus has a large databank of negative interactions feeding that anxiety. Their anxiety tells them that unstructured activities with limited adult supervision are a potential danger zone.
Those are both reasonable examples, right? But what about the anxiety-inducing holiday party, trip to the mall, or vacation? Surely that’s irrational?
Not if you’re forced to think about every social activity in terms of cost. There are many analogies for this concept: spoon theory and the social cup vs. bucket analogy are the most popular. I’ll spare you a new analogy and give you an example instead.
Last spring my nephew and his wife came to visit for a long weekend. He’s one of my favorite nephews and I was looking forward to meeting his new wife. Still, I was anxious. Having two additional people in the house for three days would mean a disrupted schedule, unfamiliar noises and smells, a loss of my precious alone time and lots and lots of talking.
The Scientist and I came up with a schedule–scheduling is essential for me to get through three days of company–and then I set about thinking of ways to conserve my resources. I volunteered to drive because I find it relaxing. We scheduled downtime for me on Saturday afternoon while everyone else went out. I suggested we visit a historical site that I knew well, because it would mean a familiar environment plus the chance to infodump in a socially acceptable way.
We had a great time. They enjoyed the places we visited and the meals I cooked. We laughed a lot and had meaningful conversations. Things couldn’t have gone better. And still, Saturday night as everyone sat around the dinner table talking for hours after the meal was finished, I found myself shaking uncontrollably.
Even with all of my planning, even though I was enjoying myself, the day’s socializing had overwhelmed me. I knew it was coming, had felt myself shutting down as the evening wore on, but I ignored the warning signs. I didn’t want to end a great day on a bad note.
Unfortunately, it’s not about what I want. Social interaction has a real physical cost for autistic people. If I don’t listen to the voice of caution in my head and limit my interactions, my body will eventually take over and limit them for me.
When I’m in a situation where I feel comfortable, I can handle longer interactions. If I have to deal with unstructured activities, unfamiliar places, new people, rapid shifts in conversation partners or topics, or any of a long list of other things I find challenging, I’ll hit my limit sooner. An hour might be all I can deal with before I start feeling a strong need to escape.
Since being diagnosed with Asperger’s, I’m getting better at “reading” myself. The anxiety, the need to escape, the withdrawal that precedes the uncontrollable shaking–these are not things I need to be cured of. They are signs that I need to take care–yellow lights to be heeded–and I’m learning to listen to them.